What Takes Vitamins Away From The Body And Increases The Risk Of Throat And Mouth Cancer
Overview of Nutrition in Cancer Care
Key Points
- Skillful diet is important for cancer patients.
- Healthy eating habits are important during and after cancer treatment.
- A registered dietitian is an important part of the healthcare squad.
- Cancer and cancer treatments may cause side effects that touch nutrition.
- Cancer and cancer treatments may cause malnutrition.
- Anorexia and cachexia are common causes of malnutrition in cancer patients.
Practiced diet is of import for cancer patients.
Nutrition is a process in which food is taken in and used by the trunk for growth, to continue the torso healthy, and to supplant tissue. Skillful nutrition is important for good health. A healthy diet includes foods and liquids that take important nutrients (vitamins, minerals, poly peptide, carbohydrates, fat, and water) the body needs.
Healthy eating habits are important during and after cancer treatment.
A diet with a focus on plant-based foods along with regular practice will help cancer patients keep a healthy body weight, maintain forcefulness, and decrease side furnishings both during and after treatment.
A registered dietitian is an of import function of the healthcare team.
A registered dietitian (or nutritionist) is a part of the team of health professionals that assistance with cancer treatment and recovery. A dietitian will work with patients, their families, and the residuum of the medical team to manage the patient'south diet during and later on cancer treatment.
Research has shown that including a registered dietitian in a patient's cancer intendance can help the patient live longer.
Cancer and cancer treatments may cause side effects that impact nutrition.
Nutrition problems are likely when tumors involve the head, cervix, esophagus, stomach, intestines, pancreas, or liver.
For many patients, the effects of cancer treatments make it difficult to eat well. Cancer treatments that affect nutrition include:
Cancer and cancer treatments may cause malnutrition.
Cancer and cancer treatments may affect sense of taste, odour, ambition, and the ability to eat plenty food or absorb the nutrients from food. This tin can cause malnutrition, which is a condition caused by a lack of key nutrients. Alcohol abuse and obesity may increase the risk of malnutrition.
Malnutrition can crusade the patient to be weak, tired, and unable to fight infection or finish cancer treatment. As a result, malnutrition tin can decrease the patient's quality of life and become life-threatening. Malnutrition may exist made worse if the cancer grows or spreads.
Eating the right amount of protein and calories is of import for healing, fighting infection, and having enough energy.
Anorexia and cachexia are mutual causes of malnutrition in cancer patients.
Anorexia is the loss of appetite or desire to eat. Information technology is a common symptom in patients with cancer. Anorexia may occur early in the disease or later, if the cancer grows or spreads. Some patients already take anorexia when they are diagnosed with cancer. Most patients who have advanced cancer will take anorexia. Anorexia is the most common cause of malnutrition in cancer patients.
Cachexia is a condition marked by weakness, weight loss, and fat and muscle loss. It is mutual in patients with tumors that affect eating and digestion. It can occur in cancer patients who are eating well, but are not storing fat and muscle because of tumor growth.
Some tumors alter the style the body uses certain nutrients. The body's utilize of protein, carbohydrates, and fat may change when tumors are in the stomach, intestines, or head and neck. A patient may seem to be eating enough, but the torso may not be able to absorb all the nutrients from the food.
Cancer patients may have anorexia and cachexia at the aforementioned time.
Furnishings of Cancer Treatment on Nutrition
Key Points
- Chemotherapy and Hormone Therapy
- Chemotherapy and hormone therapy bear on nutrition in unlike ways.
- Chemotherapy and hormone therapy cause different nutrition problems.
- Radiation Therapy
- Radiation therapy kills cells in the treatment area.
- Radiation therapy may affect nutrition.
- Surgery
- Surgery increases the body's need for nutrients and energy.
- Surgery to the caput, cervix, esophagus, stomach, or intestines may affect nutrition.
- Immunotherapy
- Immunotherapy may impact diet.
- Stem Prison cell Transplant
- Patients who receive a stem cell transplant have special nutrition needs.
Chemotherapy and Hormone Therapy
Chemotherapy and hormone therapy touch on nutrition in unlike ways.
Chemotherapy affects cells all through the body. Chemotherapy uses drugs to stop the growth of cancer cells, either by killing the cells or past stopping them from dividing. Healthy cells that normally abound and divide quickly may also be killed. These include cells in the mouth and digestive tract.
Hormone therapy adds, blocks, or removes hormones. Information technology may be used to slow or stop the growth of certain cancers. Some types of hormone therapy may cause weight gain.
Chemotherapy and hormone therapy cause unlike nutrition issues.
Side effects from chemotherapy may crusade problems with eating and digestion. When more than one chemotherapy drug is given, each drug may cause different side effects or when drugs crusade the aforementioned side effect, the side effect may be more than severe.
The following side effects are common:
- Loss of appetite.
- Nausea.
- Vomiting.
- Dry oral cavity.
- Sores in the oral fissure or throat.
- Changes in the way nutrient tastes.
- Trouble swallowing.
- Feeling total after eating a modest corporeality of food.
- Constipation.
- Diarrhea.
Patients who receive hormone therapy may need changes in their diet to forbid weight gain.
Radiation Therapy
Radiation therapy kills cells in the handling area.
Radiation therapy kills cancer cells and salubrious cells in the handling area. How severe the side effects are depends on the following:
- The part of the body that is treated.
- The total dose of radiation and how information technology is given.
Radiation therapy may affect nutrition.
Radiation therapy to any part of the digestive system has side effects that crusade diet problems. Most of the side effects begin two to three weeks after radiation therapy begins and go abroad a few weeks subsequently information technology is finished. Some side effects can proceed for months or years after treatment ends.
The following are some of the more than common side effects:
- For radiations therapy to the brain or head and neck
- Loss of appetite.
- Nausea.
- Vomiting.
- Dry mouth or thick saliva. Medication may exist given to treat a dry mouth.
- Sore oral fissure and gums.
- Changes in the way food tastes.
- Trouble swallowing.
- Pain when swallowing.
- Being unable to fully open up the mouth.
- For radiations therapy to the breast
- Loss of appetite.
- Nausea.
- Vomiting.
- Trouble swallowing.
- Pain when swallowing.
- Choking or breathing problems caused by changes in the upper esophagus.
- For radiation therapy to the abdomen, pelvis, or rectum
- Nausea.
- Vomiting.
- Bowel obstruction.
- Colitis.
- Diarrhea.
Radiation therapy may also cause tiredness, which can atomic number 82 to a decrease in appetite.
Surgery
Surgery increases the body's need for nutrients and energy.
The body needs extra energy and nutrients to heal wounds, fight infection, and recover from surgery. If the patient is malnourished before surgery, information technology may cause bug during recovery, such equally poor healing or infection. For these patients, nutrition care may begin earlier surgery.
Surgery to the head, cervix, esophagus, tum, or intestines may affect nutrition.
Most cancer patients are treated with surgery. Surgery that removes all or part of sure organs tin bear on a patient's ability to eat and digest nutrient.
The following are nutrition problems caused by surgery:
- Loss of appetite.
- Trouble chewing.
- Trouble swallowing.
- Feeling full after eating a minor amount of food.
Immunotherapy
Immunotherapy may affect nutrition.
The side effects of immunotherapy are different for each patient and the blazon of immunotherapy drug given.
The following nutrition problems are common:
- Tiredness.
- Fever.
- Nausea.
- Vomiting.
- Diarrhea.
Stalk Cell Transplant
Patients who receive a stem cell transplant have special nutrition needs.
Chemotherapy, radiation therapy, and other medicines used before or during a stem cell transplant may cause side furnishings that keep a patient from eating and digesting food as usual.
Mutual side effects include the post-obit:
- Mouth and throat sores.
- Diarrhea.
Patients who receive a stem jail cell transplant have a high risk of infection. Chemotherapy or radiation therapy given earlier the transplant decrease the number of white blood cells, which fight infection. It is of import that these patients learn about condom food handling and avoid foods that may crusade infection.
After a stem cell transplant, patients are at risk for acute or chronic graft-versus-host disease (GVHD). GVHD may bear upon the alimentary canal or liver and change the patient's ability to eat or absorb nutrients from food.
Diet Assessment in Cancer Intendance
Fundamental Points
- The healthcare team may ask questions almost diet and weight history.
- Counseling and diet changes are made to improve the patient'south nutrition.
- The goal of nutrition therapy for patients who accept avant-garde cancer depends on the overall plan of care.
The healthcare team may enquire questions about diet and weight history.
Screening is used to look for health issues that bear on the adventure of poor diet. This can help find out if the patient is likely to become malnourished, and if diet therapy is needed.
The healthcare squad may ask questions about the post-obit:
- Weight changes over the past year.
- Changes in the corporeality and blazon of food eaten.
- Problems that take afflicted eating, such as loss of appetite, nausea, vomiting, diarrhea, constipation, mouth sores, dry out rima oris, changes in taste and smell, or pain.
- Ability to walk and do other activities of daily living (dressing, getting into or out of a bed or chair, taking a bath or shower, and using the toilet).
A physical exam is done to cheque the body for full general health and signs of disease. The patient is checked for signs of loss of weight, fat, and muscle, and for fluid buildup in the torso.
Counseling and diet changes are made to improve the patient'south nutrition.
A registered dietitian tin work with patients and their families to counsel them on ways to amend the patient's nutrition. The registered dietitian gives care based on the patient's nutrition and diet needs. Changes to the diet are made to help subtract symptoms from cancer or cancer treatment. These changes may be in the types and corporeality of nutrient, how often a patient eats, and how food is eaten (for case, at a certain temperature or taken with a harbinger).
A registered dietitian works with other members of the healthcare team to check the patient'due south nutritional health during cancer handling and recovery. In addition to the dietitian, the healthcare team may include the following:
The goal of nutrition therapy for patients who accept advanced cancer depends on the overall plan of intendance.
The goal of nutrition therapy in patients with avant-garde cancer is to give patients the all-time possible quality of life and command symptoms that cause distress.
Patients with avant-garde cancer may be treated with anticancer therapy and palliative intendance, palliative intendance alone, or may be in hospice care. Diet goals will be different for each patient. Some types of handling may exist stopped if they are not helping the patient.
Equally the focus of care goes from cancer treatment to hospice or end-of-life care, nutrition goals may become less aggressive, and a change to intendance meant to keep the patient as comfy as possible. See the Nutrition Needs at Finish of Life section for more data on nutrition at the finish of life.
Treatment of Symptoms
Key Points
- Anorexia
- Nausea
- Vomiting
- Dry Rima oris
- Mouth Sores
- Taste Changes
- Sore Throat and Trouble Swallowing
- Lactose Intolerance
- Weight Proceeds
When side furnishings of cancer or cancer treatment bear upon normal eating, changes tin can be made to assist the patient get the nutrients they demand. Eating foods that are high in calories, poly peptide, vitamins, and minerals is important. Meals should be planned to run into the patient'southward nutrition needs and tastes in nutrient.
The following are some of the more common symptoms caused by cancer and cancer treatment and ways to treat or control them.
Anorexia
The following may assist cancer patients who have anorexia (loss of ambition or desire to swallow):
- Swallow foods that are high in protein and calories. The post-obit are high-protein food choices:
- Beans.
- Chicken.
- Fish.
- Meat.
- Yogurt.
- Eggs.
- Add together extra poly peptide and calories to food, such as using poly peptide-fortified milk.
- Eat high-poly peptide foods showtime in your repast when your appetite is strongest.
- Sip just small amounts of liquids during meals.
- Drink milkshakes, smoothies, juices, or soups if you do not feel like eating solid foods.
- Swallow foods that smell good.
- Try new foods and new recipes.
- Try blenderized drinks that are high in nutrients (check with your dr. or registered dietitian first).
- Eat small meals and healthy snacks often throughout the mean solar day.
- Consume larger meals when you feel well and are rested.
- Swallow your largest meal when yous feel hungriest, whether at breakfast, tiffin, or dinner.
- Make and store modest amounts of favorite foods and so they are ready to eat when y'all are hungry.
- Be as active as possible then that you lot volition have a good appetite.
- Brush your teeth and rinse your rima oris to salvage symptoms and aftertastes.
- Talk to your doctor or registered dietitian if you have eating problems such as nausea, airsickness, or changes in how foods gustation and odor.
If these diet changes do not help with the anorexia, tube feedings may be needed and so that y'all will become plenty nutrients each day.
Medicines may be given to increment appetite. See the Medicines to Treat Loss of Appetite and Weight Loss department for more information.
Nausea
The post-obit may assist cancer patients command nausea:
- Choose foods that appeal to you. Practise non force yourself to eat food that makes y'all feel sick. Do not eat your favorite foods, to avert linking them to being sick.
- Eat foods that are banal, soft, and easy-to-digest, rather than heavy meals.
- Eat dry out foods such as crackers, bread sticks, or toast throughout the day.
- Eat foods that are like shooting fish in a barrel on your stomach, such as white toast, obviously yogurt, and clear goop.
- Eat dry toast or crackers before getting out of bed if you take nausea in the morning time.
- Eat foods and drink liquids at room temperature (not as well hot or besides cold).
- Slowly sip liquids throughout the twenty-four hours.
- Suck on difficult candies such as peppermints or lemon drops if your mouth has a bad gustatory modality.
- Stay away from food and drink with strong smells.
- Swallow v or 6 minor meals every day instead of 3 large meals.
- Sip on only pocket-size amounts of liquid during meals to avoid feeling total or swollen.
- Do not skip meals and snacks. An empty breadbasket may brand your nausea worse.
- Rinse your mouth before and after eating.
- Don't eat in a room that has cooking odors or that is very warm. Proceed the living space at a comfortable temperature and well-ventilated.
- Sit up or lie with your caput raised for one hour later on eating.
- Plan the best times for y'all to eat and drink.
- Relax before each cancer treatment.
- Wear clothes that are loose and comfortable.
- Go along a record of when y'all feel nausea and why.
- Talk with your doctor about using antinausea medicine.
Vomiting
The post-obit may help cancer patients control airsickness:
- Practise not eat or drink anything until the vomiting stops.
- Drink small amounts of articulate liquids afterward vomiting stops.
- After yous are able to potable clear liquids without vomiting, drinkable liquids such every bit strained soups, or milkshakes, that are piece of cake on your stomach.
- Consume 5 or half dozen small meals every day instead of 3 large meals.
- Sit upright and bend forward afterward airsickness.
- Ask your doc to club medicine to prevent or control vomiting.
Dry out Oral cavity
The following may help cancer patients with a dry mouth:
- Eat foods that are piece of cake to swallow.
- Moisten nutrient with sauce, gravy, or salad dressing.
- Eat foods and drinks that are very sweet or tart, such every bit lemonade, to help make more saliva.
- Chew gum or suck on hard candy, ice pops, or ice chips.
- Sip water throughout the twenty-four hour period.
- Do non drink any blazon of alcohol, beer, or wine.
- Practice not eat foods that can hurt your mouth (such as spicy, sour, salty, difficult, or crunchy foods).
- Continue your lips moist with lip balm.
- Rinse your mouth every 1 to two hours. Do not use mouthwash that contains alcohol.
- Do not use tobacco products and avert second manus smoke.
- Inquire your doctor or dentist about using bogus saliva or similar products to coat, protect, and moisten your oral cavity and pharynx.
Mouth Sores
The following can help patients who take oral cavity sores:
- Eat soft foods that are easy to chew, such as milkshakes, scrambled eggs, and custards.
- Cook foods until soft and tender.
- Cut food into modest pieces. Apply a blender or food processor to make nutrient shine.
- Suck on water ice chips to numb and soothe your mouth.
- Eat foods common cold or at room temperature. Hot foods tin can hurt your mouth.
- Drink with a harbinger to move liquid past the painful parts of your mouth.
- Utilise a small spoon to assist you lot accept smaller bites, which are easier to chew.
- Stay abroad from the following:
- Citrus foods, such as oranges, lemons, and limes.
- Spicy foods.
- Tomatoes and ketchup.
- Salty foods.
- Raw vegetables.
- Sharp and crunchy foods.
- Drinks with booze.
- Do not use tobacco products.
- Visit a dentist at least 2 weeks before starting immunotherapy, chemotherapy, or radiation therapy to the head and neck.
- Cheque your rima oris each twenty-four hour period for sores, white patches, or puffy and red areas.
- Rinse your mouth iii to 4 times a day. Mix ¼ teaspoon blistering soda, ⅛ teaspoon salt, and ane cup warm water for a mouth rinse. Do not use mouthwash that contains booze.
- Do non utilize toothpicks or other sharp objects.
Taste Changes
The following may help cancer patients who have gustatory modality changes:
- Eat poultry, fish, eggs, and cheese instead of crimson meat.
- Add together spices and sauces to foods (marinate foods).
- Swallow meat with something sweetness, such as cranberry sauce, jelly, or applesauce.
- Effort tart foods and drinks.
- Employ sugar-free lemon drops, mucilage, or mints if there is a metal or bitter taste in your mouth.
- Utilize plastic utensils and do not drink directly from metal containers if foods take a metal taste.
- Endeavor to eat your favorite foods, if you lot are not nauseated. Try new foods when feeling your best.
- Observe nonmeat, high-protein recipes in a vegetarian or Chinese cookbook.
- Chew food longer to permit more than contact with taste buds, if food tastes wearisome but not unpleasant.
- Keep foods and drinks covered, potable through a straw, turn a kitchen fan on when cooking, or cook outdoors if smells bother you lot.
- Brush your teeth and take intendance of your mouth. Visit your dentist for checkups.
Sore Throat and Trouble Swallowing
The post-obit may help cancer patients who have a sore throat or trouble swallowing:
- Eat soft foods that are like shooting fish in a barrel to chew and swallow, such as milkshakes, scrambled eggs, oatmeal, or other cooked cereals.
- Eat foods and drinks that are high in protein and calories.
- Moisten food with gravy, sauces, goop, or yogurt.
- Stay abroad from the following foods and drinks that can burn or scratch your throat:
- Hot foods and drinks.
- Spicy foods.
- Foods and juices that are high in acrid.
- Abrupt or crunchy foods.
- Drinks with alcohol.
- Cook foods until soft and tender.
- Cut food into pocket-size pieces. Employ a blender or food processor to make nutrient shine.
- Drink with a harbinger.
- Eat 5 or 6 small meals every twenty-four hour period instead of 3 large meals.
- Sit down upright and bend your head slightly forward when you consume or drinkable, and stay upright for at least 30 minutes after eating.
- Do not apply tobacco.
- Talk to your doctor about tube feedings if you lot cannot eat plenty to stay strong.
Lactose Intolerance
The following may help patients who accept symptoms of lactose intolerance:
- Utilize lactose-free or low-lactose milk products. Virtually grocery stores carry food (such equally milk and ice cream) labeled "lactose costless" or "low lactose."
- Choose milk products that are low in lactose, similar difficult cheeses (such every bit cheddar) and yogurt.
- Attempt products made with soy or rice (such as soy and rice milk and frozen desserts). These products practise not comprise lactose.
- Avoid only the dairy products that give yous problems. Eat small portions of dairy products, such as milk, yogurt, or cheese, if yous tin can.
- Try nondairy drinks and foods with calcium added.
- Consume calcium-rich vegetables, such as broccoli and greens.
- Accept lactase tablets when eating or drinking dairy products. Lactase breaks down lactose and then it is easier to digest.
- Set up your own low-lactose or lactose-free foods.
Weight Proceeds
The following may help cancer patients prevent weight proceeds:
- Consume a lot of fruits and vegetables.
- Eat foods that are loftier in cobweb, such as whole-grain breads, cereals, and pasta.
- Choose lean meats, such equally lean beef, pork trimmed of fat, and poultry (such as craven or turkey) without pare.
- Cull low-fat milk products.
- Eat less fat (consume just small-scale amounts of butter, mayonnaise, desserts, and fried foods).
- Cook with low-fatty methods, such as broiling, steaming, grilling, or roasting.
- Eat less salt.
- Consume foods that yous enjoy and then y'all experience satisfied.
- Swallow simply when hungry. Consider counseling or medicine if you eat because of stress, fearfulness, or low. If you eat because you are bored, find activities y'all enjoy.
- Consume smaller amounts of food at meals.
- Exercise daily.
- Talk with your doctor earlier going on a diet to lose weight.
Types of Nutrition Support
Cardinal Points
- Nutrition back up helps patients who cannot eat or digest food normally.
- Nutrition support can be given in different ways.
- Enteral Nutrition
- Enteral nutrition is also chosen tube feeding.
- Parenteral Nutrition
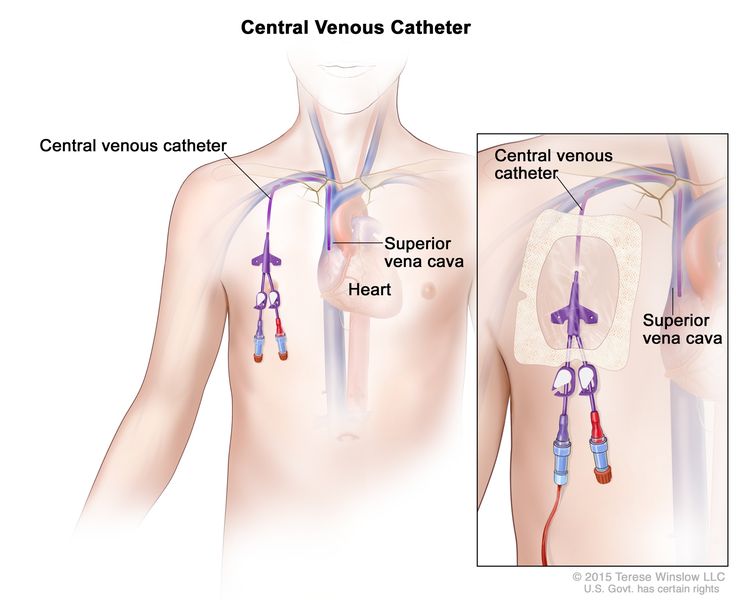
- Parenteral nutrition carries nutrients directly into the blood stream.
- The catheter may be placed into a vein in the chest or in the arm.
Nutrition support helps patients who cannot eat or digest food normally.
It is best to take in food past oral fissure whenever possible. Some patients may non exist able to take in enough food by mouth because of problems from cancer or cancer treatment.
Nutrition support can be given in different ways.
In addition to counseling past a dietitian, and changes to the diet, diet therapy includes nutritional supplement drinks, and enteral and parenteral nutrition back up. Nutritional supplement drinks assistance cancer patients get the nutrients they need. They provide energy, poly peptide, fatty, carbohydrates, cobweb, vitamins, and minerals. They are not meant to be the patient'due south only source of nutrition.
A patient who is not able to take in the right amount of calories and nutrients by mouth may be fed using the following:
- Enteral nutrition: Nutrients are given through a tube inserted into the breadbasket or intestines.
- Parenteral nutrition: Nutrients are infused into the bloodstream.
Nutrition support can improve a patient'due south quality of life during cancer treatment, simply may cause problems that should exist considered before making the decision to use it. The patient and healthcare team should discuss the harms and benefits of each type of diet back up. (See the Nutrition Needs at Terminate of Life department for more data on the apply of nutrition support at the end of life.)
Enteral Nutrition
Enteral nutrition is too chosen tube feeding.
Enteral diet gives the patient nutrients in liquid form (formula) through a tube that is placed into the stomach or pocket-size intestine. The post-obit types of feeding tubes may be used:
- A nasogastric tube is inserted through the olfactory organ and down the throat into the tummy or small intestine. This is used when enteral diet is simply needed for a few weeks.
- A gastrostomy tube is inserted into the stomach or a jejunostomy tube is inserted into the small intestine through an opening made on the outside of the belly. This is usually used for long-term enteral feeding or for patients who cannot employ a tube in the nose and throat.
The blazon of formula used is based on the specific needs of the patient. There are formulas for patients who have special health conditions, such as diabetes, or other needs, such as religious or cultural diets.
Parenteral Nutrition
Parenteral diet carries nutrients directly into the blood stream.
Parenteral nutrition is used when the patient cannot take food past mouth or by enteral feeding. Parenteral feeding does not use the tummy or intestines to assimilate food. Nutrients are given to the patient directly into the blood, through a catheter inserted into a vein. These nutrients include proteins, fats, vitamins, and minerals.
The catheter may be placed into a vein in the breast or in the arm.
A central venous access catheter is placed beneath the pare and into a large vein in the upper chest. The catheter is put in place past a surgeon. This type of catheter is used for long-term parenteral feeding.
A peripheral venous catheter is placed into a vein in the arm. A peripheral venous catheter is put in identify by trained medical staff. This type of catheter is commonly used for brusque-term parenteral feeding for patients who practice not have a central venous access catheter.
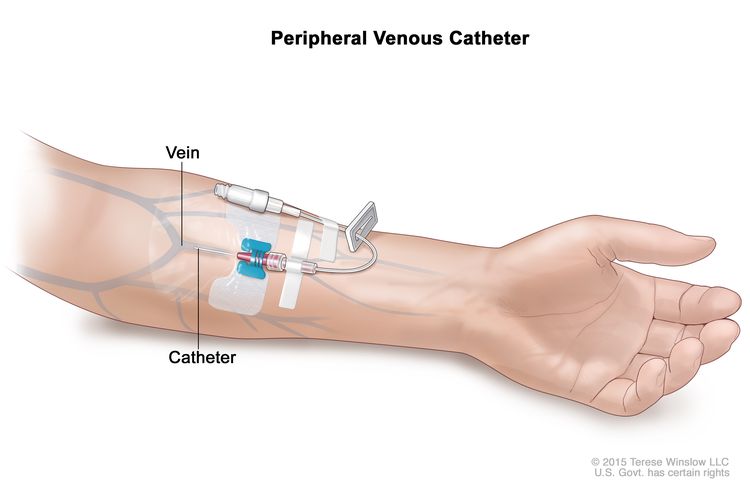
The patient is checked often for infection or bleeding at the place where the catheter enters the body.
Medicines to Treat Loss of Appetite and Weight Loss
Key Points
- Medicine may be given with nutrition therapy to care for loss of appetite and weight loss.
- Different types of medicine may be used to treat loss of appetite and weight loss.
Medicine may exist given with diet therapy to treat loss of appetite and weight loss.
Information technology is important that cancer symptoms and side effects that affect eating and crusade weight loss are treated early on. Both nutrition therapy and medicine can aid lessen the furnishings that cancer and its treatment have on weight loss.
Different types of medicine may exist used to treat loss of appetite and weight loss.
Medicines that better appetite and cause weight proceeds, such as prednisone and megestrol, may be used to care for loss of appetite and weight loss. Studies have shown that the upshot of these medicines may non terminal long or in that location may be no effect. Treatment with a combination of medicines may work better than handling with one medicine. Patients who are treated with a combination of medicines may accept more side effects.
Nutrition Needs at End of Life
Key Points
- Nutrition needs change at finish of life.
- Patients and families decide how much diet and fluids will be given at the end of life.
Nutrition needs modify at end of life.
For patients at the terminate of life, the goals of nutrition therapy are focused on relieving symptoms rather than getting enough nutrients.
Mutual symptoms that can occur at the finish of life include the following:
- Anorexia (loss of appetite).
- Dry rima oris.
- Swallowing bug.
- Nausea.
- Vomiting.
Patients who have bug swallowing may find it easier to consume thick liquids than sparse liquids.
Patients oftentimes do not feel much hunger at all and may want very petty food. Sips of h2o, ice fries, and mouth intendance tin can decrease thirst in the final few days of life. Good communication with the healthcare team is important to empathise the patient'south changes in diet needs.
Patients and families decide how much nutrition and fluids will be given at the finish of life.
Cancer patients and their caregivers take the right to make informed decisions. The patient's religious and cultural preferences may impact their decisions. The healthcare team may work with the patient's religious and cultural leaders when making decisions. The healthcare team and a registered dietitian can explain the benefits and risks of using diet support for patients at the end of life. In most cases, in that location are more harms than benefits.
The risks of nutrition support at the end of life include the following:
- Sepsis (bacteria or their toxins in the blood or tissues) with the use of parenteral diet.
- Aspiration (the adventitious animate in of food or fluid into the lungs) with the use of enteral nutrition.
- Sores and breakdown of the pare where the enteral feeding tube is inserted.
- Diarrhea with the use of enteral and parenteral diet.
- Complications acquired by fluid overload (a condition where there is too much fluid in the blood) with the employ of enteral and parenteral diet.
Nutrition Trends in Cancer
Key Points
- Some cancer patients effort special diets to improve their prognosis.
- Some cancer patients may take dietary supplements.
Some cancer patients try special diets to meliorate their prognosis.
Cancer patients may try special diets to brand their treatment work meliorate, prevent side effects from handling, or to treat the cancer itself. Withal, for most of these special diets, in that location is no evidence that shows they piece of work.
Vegetarian or vegan diet
Information technology is non known if following a vegetarian or vegan diet tin can help side effects from cancer treatment or the patient'southward prognosis. If the patient already follows a vegetarian or vegan nutrition, there is no evidence that shows they should switch to a different nutrition.
Macrobiotic diet
A macrobiotic diet is a loftier-carbohydrate, depression-fat, plant-based nutrition. No studies have shown that this diet will assist cancer patients.
Ketogenic diet
A ketogenic diet limits carbohydrates and increases fat intake. The purpose of the nutrition is to subtract the amount of glucose (sugar) the tumor cells can use to abound and reproduce. Information technology is a hard diet to follow because exact amounts of fats, carbohydrates and proteins are needed. Yet, the nutrition is safe.
Several clinical trials are recruiting glioblastoma patients to study whether a ketogenic nutrition affects glioblastoma tumor activity. Patients with glioblastoma who want to start a ketogenic diet should talk to their doctor and work with a registered dietitian. Yet, it is not withal known how the diet will affect the tumor or its symptoms.
Similarly, a written report comparing the ketogenic diet to a loftier-cobweb, depression fatty diet in women with ovarian cancer or endometrial cancer found that the ketogenic diet was safe and acceptable. There is not plenty evidence to know how the ketogenic diet will bear on ovarian or endometrial tumors or their symptoms.
Some cancer patients may accept dietary supplements.
A dietary supplement is a production that is added to the diet. It is unremarkably taken by mouth, and usually has ane or more than dietary ingredients. Cancer patients may take dietary supplements to improve their symptoms or care for their cancer.
Vitamin C
Vitamin C is a nutrient that the body needs in small amounts to role and stay good for you. Information technology helps fight infection, heal wounds, and keep tissues salubrious. Vitamin C is establish in fruits and vegetables. It can also be taken every bit a dietary supplement.
See the PDQ summary on Loftier-Dose Vitamin C for more data virtually the apply of intravenous high-dose vitamin C equally treatment for people with cancer.
Probiotics
Probiotics are live microorganisms used as dietary supplements to help with digestion and normal bowel part. They may besides help keep the gastrointestinal tract healthy.
Studies have shown that taking probiotics during radiation therapy and chemotherapy tin can help prevent diarrhea acquired by those treatments. This is true for patients who receive radiations therapy to the abdomen. Cancer patients who are receiving radiation therapy to the abdomen or chemotherapy that is known to cause diarrhea may exist helped past probiotics. Similarly, studies are looking at potential benefits of taking probiotics for cancer patients who are receiving immunotherapy.
Melatonin
Melatonin is a hormone fabricated by the pineal gland (tiny organ near the eye of the brain). Melatonin helps control the trunk's sleep bike. It can also exist made in a laboratory and taken as a dietary supplement.
Several small studies have shown that taking a melatonin supplement with chemotherapy and/or radiation therapy for handling of solid tumors may be helpful. It may assist reduce side effects of treatment. Melatonin does not appear to have side effects.
Oral glutamine
Oral glutamine is an amino acid that is being studied for the treatment of diarrhea and mucositis (inflammation of the lining of the digestive system, ofttimes seen every bit mouth sores) caused past chemotherapy or radiation therapy. Oral glutamine may assistance prevent mucositis or get in less severe.
Cancer patients who are receiving radiation therapy to the abdomen may benefit from oral glutamine. Oral glutamine may reduce the severity of diarrhea. This can help the patients keep with their treatment plan.
To Learn More than About Diet and Cancer Care
National Cancer Institute
For information from the National Cancer Plant (NCI) nigh nutrition and cancer treatment, see Side Furnishings.
Organizations
For general nutrition data and other resources, encounter the following:
- United States Section of Agriculture
- Academy of Nutrition and Dietetics
- American Botanical Council
- American Cancer Society
- American Institute for Cancer Research
- American Society for Parenteral and Enteral Nutrition
- National Center for Complementary and Integrative Health (NCCIH)
- 888-644-6226 (NCCIH Clearinghouse)
- 866-464-3615 (cost costless TTY)
- nccih.nih.gov
- Role of Dietary Supplements
Books
- American Cancer Society's Healthy Eating Cookbook: A Celebration of Food, Friends, and Salubrious Living. 3rd ed. Atlanta, GA: The American Cancer Society, 2005.
- Bloch A, Cassileth BR, Holmes Md, Thomson CA, eds.: Eating Well, Staying Well During and After Cancer. Atlanta, GA: American Cancer Club, 2004.
- Ghosh K, Carson L, and Cohen East: Betty Crocker'due south Living with Cancer Cookbook: Easy Recipes and Tips Through Treatment and Beyond. New York, NY: Hungry Minds, 2002.
- Weihofen DL, Robbins J, Sullivan PA: Easy-to-Eat, Like shooting fish in a barrel-to-Chew Cookbook: Over 150 Tasty and Nutritious Recipes for People Who Have Difficulty Swallowing. New York, NY: John Wiley & Sons, Inc., 2002.
- Wilson JR: I-Can't-Chew Cookbook: Delicious Soft Nutrition Recipes for People with Chewing, Swallowing, or Dry Mouth Disorders. Alameda, Calif: Hunter House Inc., 2003.
Electric current Clinical Trials
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the blazon of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Virtually This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute'due south (NCI'southward) comprehensive cancer data database. The PDQ database contains summaries of the latest published data on cancer prevention, detection, genetics, treatment, supportive intendance, and complementary and alternative medicine. Most summaries come in 2 versions. The health professional versions accept detailed information written in technical linguistic communication. The patient versions are written in easy-to-understand, nontechnical linguistic communication. Both versions have cancer data that is accurate and upwards to date and most versions are also bachelor in Spanish.
PDQ is a service of the NCI. The NCI is role of the National Institutes of Health (NIH). NIH is the federal regime's eye of biomedical research. The PDQ summaries are based on an contained review of the medical literature. They are non policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current data virtually diet before, during, and afterwards cancer treatment. It is meant to inform and assistance patients, families, and caregivers. Information technology does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer handling and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new data. The date on each summary ("Updated") is the date of the most recent change.
The data in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Supportive and Palliative Intendance Editorial Lath.
Clinical Trial Information
A clinical trial is a study to reply a scientific question, such equally whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in social club to discover new and better ways to help cancer patients. During handling clinical trials, information is nerveless about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may get "standard." Patients may want to call up about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials tin can exist found online at NCI'south website. For more than data, telephone call the Cancer Information Service (CIS), NCI'due south contact eye, at ane-800-4-CANCER (1-800-422-6237).
Permission to Utilise This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely equally text. Information technology cannot exist identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI'southward PDQ cancer information summary about chest cancer prevention states the risks in the post-obit mode: [include excerpt from the summary]."
The all-time way to cite this PDQ summary is:
PDQ® Supportive and Palliative Care Editorial Board. PDQ Nutrition in Cancer Intendance. Bethesda, MD: National Cancer Found. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/about-cancer/treatment/side-effects/ambition-loss/diet-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389440]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to utilise an epitome from a PDQ summary and y'all are non using the whole summary, you must become permission from the owner. It cannot be given by the National Cancer Found. Data well-nigh using the images in this summary, forth with many other images related to cancer can exist plant in Visuals Online. Visuals Online is a collection of more than iii,000 scientific images.
Disclaimer
The information in these summaries should non be used to make decisions about insurance reimbursement. More than data on insurance coverage is available on Cancer.gov on the Managing Cancer Care folio.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can likewise be submitted to Cancer.gov through the website'due south E-mail Us.
What Takes Vitamins Away From The Body And Increases The Risk Of Throat And Mouth Cancer,
Source: https://www.cancer.gov/about-cancer/treatment/side-effects/appetite-loss/nutrition-pdq
Posted by: williamssaver1959.blogspot.com


0 Response to "What Takes Vitamins Away From The Body And Increases The Risk Of Throat And Mouth Cancer"
Post a Comment